Updated November 14, 2025 By Rim El Helou & Lamia Ghernati
🌍 November — Diabetes Awareness Month
Every November, the world comes together to shine a light on one of the most common and growing chronic conditions: diabetes.
But here’s the good news: knowledge is power. By understanding how diabetes develops and how nutrition influences it, we can take meaningful steps to prevent and manage it, for ourselves, our families, and especially our children.
In this blog, we’ll explore how parents can support their children’s well-being through balanced nutrition, smart snacking, and family-friendly meal habits.
🩸 What Is Diabetes?
Diabetes is not simply “too much sugar in the blood.”
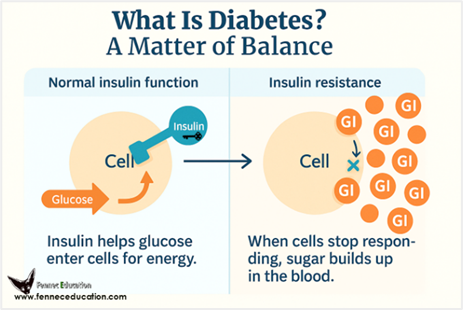
It’s a metabolic disorder in which the body struggles to regulate glucose, the main fuel that powers our cells. At the center of this balance is insulin, a hormone produced by the pancreas. Insulin acts like a key 🔑, unlocking cells so that glucose can enter and be used for energy. But its role goes far beyond that.
✨ Insulin helps maintain energy balance by:
- Storing glucose in the liver and muscles, ensuring a steady supply of energy between meals, during fasting, or while sleeping.
- while also preventing the breakdown of existing proteins, helping the body preserve its muscle strength and stores.
- Converting excess glucose into fat, stored in adipose tissue for future use.
When insulin is missing or when cells stop responding to it, a condition called insulin resistance, glucose remains in the bloodstream instead of nourishing the body.
As a result, cells are starved of energy, the body begins to break down protein and fat for fuel, and blood sugar levels rise. This state, known as hyperglycemia, can lead to medical emergencies, long-term organ damage, and, if left untreated, life-threatening complications.
But insulin is not the enemy; it’s a vital hormone that supports nearly every system in the body. Our goal is to help it function optimally through balanced nutrition, movement, and mindful living.
🔍 Type 1 vs. Type 2 Diabetes: Key Differences and Early Signs
Understanding the difference between Type 1 and Type 2 diabetes helps parents act quickly if something seems off with their child’s health. Both conditions affect how the body uses sugar (glucose) for energy, but they have different causes, risk factors, and warning signs.
1. Type 1 Diabetes: When the Body Stops Making Insulin
In Type 1 diabetes, the immune system mistakenly attacks and destroys the cells in the pancreas that produce insulin. Without insulin, glucose cannot enter the body’s cells, leading to a buildup of sugar in the bloodstream.
This form of diabetes usually appears in childhood or adolescence, with an average onset around 12 years old, though it can develop at any age. Researchers believe it is influenced by genetic factors and sometimes viral infections that trigger the immune reaction. Symptoms usually appear suddenly over days or weeks.
Common symptoms include:
- Frequent urination, especially at night
- Bedwetting in a child who was previously dry at night
- Constant thirst and dry mouth
- Extreme hunger
- Rapid, unexplained weight loss despite normal or increased appetite.
- Fatigue, weakness, and irritability
- Blurred vision
- Fruity or sweet-smelling breath (a sign of ketone buildup).
- Nausea or vomiting (can signal diabetic ketoacidosis, a medical emergency).
🩺 When to act: Type 1 diabetes can develop quickly and may lead to a serious condition called diabetic ketoacidosis (DKA). If your child shows several of these signs, contact a pediatrician immediately for blood sugar testing.
Type 1 diabetes affects about 5–10% of all people with diabetes. Since the pancreas can no longer produce insulin, treatment requires daily insulin therapy, through injections or an insulin pump, combined with blood sugar monitoring and nutritional balance.
Nutrition management focuses on:
- Synchronizing insulin doses with meal timing
- Adjusting pre-meal insulin based on carbohydrate content
- Ensuring enough energy and nutrients for growth, activity, and healing
💡 Type 1 diabetes cannot be prevented, but with education and care, children and adults can live full, healthy, and active lives.
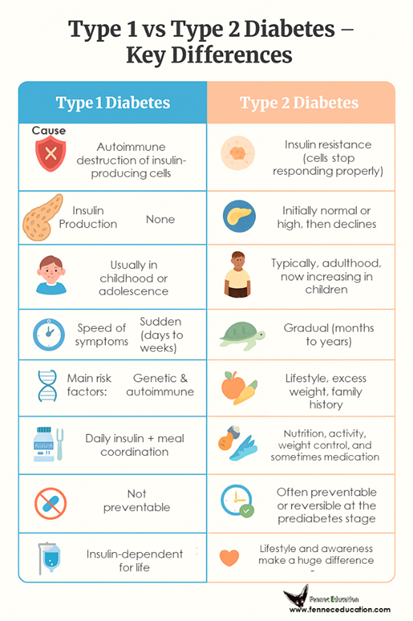
2. Type 2 Diabetes: When the Body Stops Responding to Insulin
In Type 2 diabetes, the body still makes insulin, but the cells no longer respond to it effectively. This condition, known as insulin resistance, causes glucose to remain in the blood rather than entering the cells for energy. Over time, the pancreas, which started to increase its Insulin production as a response to this resistance, may become exhausted and produce less insulin.
Traditionally, Type 2 diabetes appeared in adults over 40 years old, but with modern lifestyle changes, high-sugar diets, processed foods, and less physical activity, it is now increasingly common in children and teenagers.
Typical symptoms develop gradually and may include:
- Tiredness and lack of energy
- Increased thirst and urination
- Frequent infections, such as skin or gum infections
- Slow-healing wounds, especially on the feet or legs
- Blurred vision or mild vision changes (due to fluctuating glucose levels)
- Dark, velvety skin patches (acanthosis nigricans) on the neck, armpits, or elbows
- Tingling, numbness, or burning sensations in hands or feet (early nerve changes)
🩺 When to act: If your child shows subtle but persistent changes, it’s important to talk to the doctor and request blood tests, including the HOMA-IR test for insulin resistance.
Type 2 diabetes accounts for 90–95% of all cases. The good news is that, unlike Type 1, it can often be prevented or delayed through healthy lifestyle habits.
Medical care focuses on:
1️⃣ Regular monitoring of blood glucose and HbA1C
2️⃣ Increased physical activity, as it makes your muscles more sensitive to insulin, and improves glucose metabolism
3️⃣ Use of medication (oral drugs or insulin) when necessary
Nutrition and lifestyle care emphasize:
- A balanced diet rich in fiber, lean proteins, and healthy fats
- Limiting sugary foods and drinks
- Weight management and daily movement
- Nutrition education for families to make informed food choices
🌿 Pre-diabetes, the stage before Type 2, is a crucial warning sign. With early intervention, it can often be reversed, preventing lifelong diabetes.
🩷 Side Note: Beyond Type 1 and Type 2
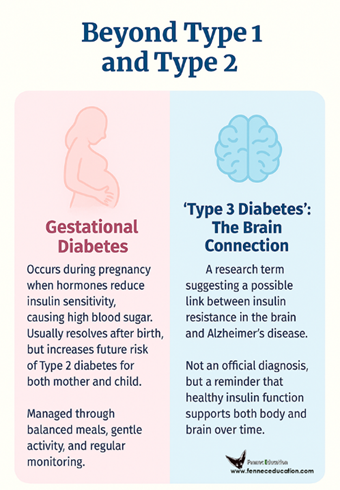
1. Gestational Diabetes: When Pregnancy Challenges Insulin Sensitivity
Gestational diabetes occurs when pregnancy hormones reduce the body’s sensitivity to insulin.
This causes blood sugar levels to rise during pregnancy, usually appearing around the second or third trimester. While it typically resolves after delivery, women who experience gestational diabetes are at greater risk of developing Type 2 diabetes later in life, and so are their children.
Prevention and care focus on:
- Regular screening and glucose testing during pregnancy
- Balanced nutrition with controlled carbohydrate portions
- Moderate, doctor-approved physical activity
🤍 With guidance, most women have healthy pregnancies and healthy babies.
2. “Type 3 Diabetes”: The Brain Connection
The term “Type 3 diabetes” is sometimes used by researchers to describe a proposed link between insulin resistance in the brain and Alzheimer’s disease.
While not officially recognized as a type of diabetes, this idea highlights how metabolic health and brain function are interconnected. Insulin plays an important role in brain cell health, memory, and cognition, so when it doesn’t work properly, it may contribute to neurodegenerative changes.
🧠 This emerging area of research reminds us that supporting insulin function isn’t only about blood sugar, it’s also about protecting long-term brain health.
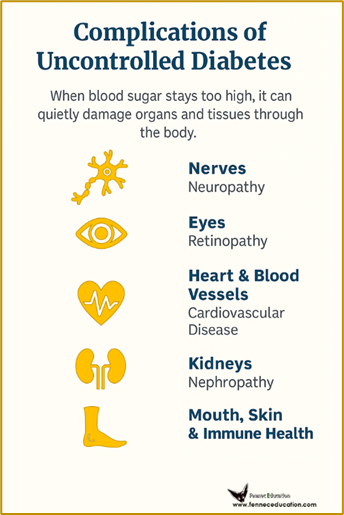
💔 Why It Matters: Complications of Uncontrolled Diabetes
Diabetes is often misunderstood as “just high blood sugar.” In reality, when blood glucose remains elevated for too long, it silently damages blood vessels, nerves, and vital organs. Understanding these complications reminds us that good management is about protecting the whole body, not just lowering numbers.
1. Neuropathy : When Nerves Suffer
High blood sugar over time damages the tiny blood vessels that supply the nerves, especially in the hands and feet. This can cause tingling, numbness, burning pain, or loss of sensation, which may make injuries go unnoticed.
If untreated, neuropathy can lead to balance problems, infections, or even limb ulcers that, in advanced stages, may require amputation. Regular foot checks, good glucose control, and physical activity help protect nerve health.
2. Retinopathy: The Eyes at Risk
The delicate blood vessels in the retina are very sensitive to glucose levels. Prolonged hyperglycemia can cause them to leak or close off, leading to blurred vision, floaters, or vision loss.
Early screening is vital, eye exams can detect changes before vision is affected.
💡 A balanced diet rich in antioxidants (vitamins A, C, and E, plus omega-3s) also supports eye health.
3. Nephropathy: Protecting the Kidneys
The kidneys filter waste and excess glucose from the blood. When blood sugar and blood pressure stay high, these filters (nephrons) become damaged, causing protein to leak into urine. Over time, this may progress to chronic kidney disease or kidney failure, a very serious disease.
Staying hydrated, moderating salt and protein intake, and controlling blood sugar are key to prevention.
4. Cardiovascular Disease: The Heart Connection
Diabetes accelerates atherosclerosis (the buildup of plaque in arteries), increasing the risk of heart attack, stroke, and poor circulation. Managing cholesterol, staying active, eating heart-healthy fats, and not smoking all reduce this risk.
❤️ Heart care and glucose care go hand in hand.
5. Infections: A Hidden Danger
Elevated blood sugar weakens immune defenses and provides a growth environment for bacteria and fungi. This leads to slow-healing wounds, urinary tract infections, and skin or gum infections.
Good hygiene, balanced nutrition, and stable glucose levels are the best defenses.
✨ In Summary
Diabetes affects the entire body, but every healthy habit counts. Keeping blood sugar in range protects the nerves, kidneys, heart, eyes, and overall quality of life.
⚠️ Diabetes is not just a matter of taking insulin; it’s a lifelong condition that requires attention, balance, and care.
🥗 The Power of Nutrition: Prevention and Management
Nutrition plays a central role in both preventing diabetes and managing it once diagnosed. Food doesn’t just nourish, it sends powerful signals to our metabolism, hormones, and energy balance.
What, when, and how we eat directly influence insulin sensitivity, blood sugar control, and even inflammation in the body. The goal is not to follow a “diabetic diet,” but to build a balanced and sustainable way of eating that supports stable energy, good mood, and long-term health.
🌾 1. Choose Whole, Unprocessed Foods
Whole foods: fruits, vegetables, legumes, nuts, seeds, and whole grains provide fiber, vitamins, and minerals that help slow glucose absorption and keep you fuller for longer. They prevent sudden sugar spikes and promote smooth, steady energy.
💡 Aim for variety and color; each shade brings unique antioxidants that protect the heart, eyes, and nerves.
🍞 2. Prioritize Smart Carbohydrates
Carbohydrates aren’t the enemy, but quality and quantity matter. Choose low glycemic index (GI) options such as oats, brown rice, lentils, chickpeas, sweet potatoes, and quinoa. These foods release glucose gradually, giving your body time to respond with appropriate insulin levels.
Avoid refined carbs like white bread, pastries, sugary drinks, and sweets, which cause rapid spikes followed by energy crashes.
🥑 3. Include Healthy Fats
Healthy fats improve insulin sensitivity and support heart health. Focus on unsaturated fats from olive oil, avocado, nuts, seeds, and fatty fish (like salmon, sardines, or mackerel). Limit trans fats and highly processed oils often found in packaged snacks and fast food.
💧 Remember — fats don’t raise blood sugar, but the right kinds help the body use insulin more effectively.
🍗 4. Add Lean Proteins
Protein supports muscle maintenance, slows digestion, and helps control hunger. Include a mix of lean animal and plant-based sources: eggs, poultry, fish, beans, lentils, tofu, or yogurt.
Balanced protein intake also helps regulate blood sugar by moderating the effect of carbohydrates on glucose levels.
🍽️ 5. Building a Balanced Plate: The Diabetes-Friendly Way for the Whole Family
Try the “Healthy Plate” method:
- 🥦 ½ vegetables or salad (fiber and antioxidants)
- 🍗 ¼ lean protein (meat, fish, tofu, legumes)
- 🌾 ¼ whole grains or complex carbs (brown rice, quinoa, whole wheat)
Add a drizzle of healthy fat like olive oil or a few nuts to complete the plate.
👉🏼 Eating balanced meals every 3–4 hours help maintain consistent glucose levels and prevents overeating.
👉🏼 Make meals colorful and engaging. Involve children in grocery shopping and cooking, which teaches them to make better choices early.
👉🏼 Family meals encourage bonding, mindful eating, and consistency, powerful tools for lifelong health.
🕐 6. Be Mindful of Timing
When and how often we eat can be just as important as what we eat. Spacing meals evenly throughout the day supports better insulin action, helps maintain steady energy, and prevents blood sugar spikes and crashes.
However, eating late at night can disturb the body’s natural rhythm. Our metabolism naturally slows in the evening, making it harder to process food efficiently. Eating large or high-sugar meals late at night can lead to higher blood sugar levels, insulin resistance, and, over time, an increased risk of weight gain and diabetes.
If you’re hungry before bed, a light, balanced snack like a small yogurt, a handful of nuts, or a piece of fruit is usually better than skipping or overeating.
💡 Late-night snacking isn’t always harmful, but what and when you eat matters. Choose smart options and, if you have diabetes, check your glucose levels to keep them stable overnight.
💡When personalized, fasting can help improve insulin sensitivity and support better blood sugar control. However, it’s important to do it safely and with professional guidance, as fasting without proper balance may cause nutrient deficiencies or unstable glucose levels.
💧 7. Hydrate Wisely
Water is the best drink for everyone, and especially important for those with diabetes.
Staying hydrated helps the kidneys flush out excess glucose and prevents dehydration from frequent urination.
👉🏼 Avoid sugary beverages, fruit juices, and sweetened teas, even “natural” ones, as they quickly raise blood sugar.

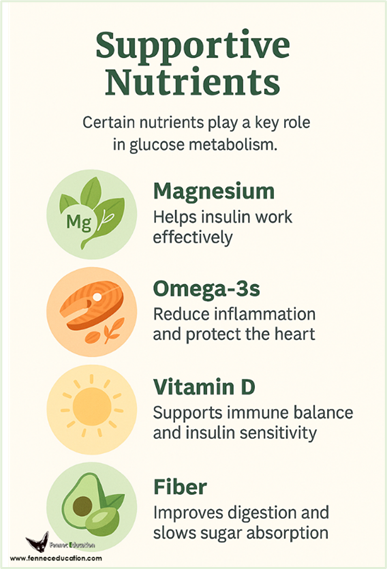
🌿 Supportive Nutrients
Certain nutrients play a key role in glucose metabolism:
- Magnesium: helps insulin work effectively (found in leafy greens, cocoa, nuts, and seeds).
- Omega-3 fatty acids: reduce inflammation and protect the heart (found in fatty fish, flaxseeds, and walnuts).
- Vitamin D: supports immune balance and insulin sensitivity.
- Fiber: improves digestion, lowers cholesterol, and slows sugar absorption.
💡 A balanced diet usually provides what you need, but your doctor may recommend supplementation if deficiencies are detected.
🍎 Smart Snacking for Kids: Healthy Alternatives to Sugary Treats
Children love snacks and snacks can love them back! The goal isn’t to remove treats, but to choose options that fuel energy and balance blood sugar instead of causing crashes and cravings.
- Water, sparkling water with lemon, or milk
- Apple or banana slices + nut butter or a few dark-chocolate chips
- Yogurt with berries
- Veggie sticks, cucumber slices, or cherry tomatoes with hummus or guacamole
- Popcorn, nuts, or whole-grain crackers
- Homemade fruit popsicles
- Oatmeal topped with cinnamon and fresh fruit
💡 Pairing fiber, protein, and healthy fat helps kids feel satisfied for longer and avoids sudden sugar crashes.
🧺 Snack Planning Tips for Parents
• Offer snacks at regular times instead of grazing all day. Structure helps appetite regulation.
• Keep healthy options visible and accessible: fruit bowls, cut-up veggies, or small yogurt pots in the fridge.
• Involve children in preparing snacks; it turns nutrition into play and builds awareness.
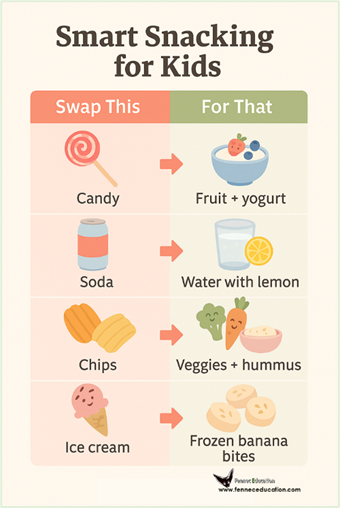
• For school or outings, pack portable options like nuts, whole-grain crackers, cheese sticks, or boiled eggs.
💛 Living with Diabetes: Helping Children Adapt and Thrive
A diabetes diagnosis can feel overwhelming for both children and parents, but with the right support, kids with diabetes can live full, active, and happy lives. The goal is not to limit them, but to help them feel confident and capable of managing their condition within their daily environment; at home, school, and with friends.
👩🏻⚕️1. The Dietitian: Education Comes First
The journey begins with education and support. After consulting your diabetologist, one of the first essential steps is to meet a registered dietitian, who will:
- Teach families to count carbohydrates and calories.
- Explain how to monitor blood sugar using a glucose device.
- Guide parents on adjusting meals and snacks based on readings and insulin needs.
Beyond numbers and food, this early education builds confidence and understanding, helping children and parents see diabetes not as a restriction, but as a manageable part of daily life.
🏠 2. At Home: Building Confidence and Routine
- Create a stable routine: Regular meal times, balanced snacks, and daily physical activity help regulate blood sugar and reduce stress.
- Involve your child: Let them help plan meals, count carbs, or choose healthy snacks, it gives them a sense of control and independence.
- Normalize it: Avoid making diabetes feel like a punishment. Keep discussions open, positive, and celebrate small successes in self-care.
- Stay prepared: Keep glucose meters, snacks, and insulin supplies easily accessible so your child feels secure and supported.
💡 Consistency builds confidence and confidence builds resilience.
🏫 3. At School: Partnering with Teachers and Staff
- Communicate early: Meet with teachers, the school nurse, and staff to explain your child’s needs, when they might need to eat, test blood sugar, or take insulin.
- Provide a care plan: Write clear instructions for recognizing and managing low or high blood sugar.
- Encourage inclusion: Children with diabetes can and should participate fully in classes, sports, and events. With good planning, they can join safely and confidently.
🫶 Teamwork between parents, teachers, and healthcare professionals helps create a safe and supportive school environment.
🤝 Social and Emotional Support
- Talk about feelings: Some children may feel different or embarrassed. Listen to their worries and reassure them that many other children live well with diabetes.
- Build a support network: Connect with other families or local diabetes associations, sharing experiences helps both parents and kids feel less alone.
- Empower, don’t overprotect: Teach your child to recognize signs of low blood sugar (like dizziness or sweating) and to ask for help when needed.
💬 Confidence grows when children understand their bodies and trust themselves.
🎂 4. Diabetes and Birthday Parties: Finding the Right Balance
Birthday parties are a big part of childhood: cake, treats, and fun with friends. For children with diabetes, these moments don’t have to mean missing out. With a little planning, they can join in safely and enjoy every celebration.
💡 Before the Party: Plan Ahead
- Talk to the host or parent: Let them know your child has diabetes and may need to check blood sugar or eat a snack at certain times. Most parents are understanding and happy to help.
- Plan meals and timing: If possible, serve a balanced meal before the party. A mix of protein and fiber helps prevent sugar spikes from party sweets later.
- Pack smart snacks: Bring along a small kit: healthy treats (like fruit, nuts, or a whole-grain bar), glucose tablets, and water, so your child always has safe options.
🍰 During the Party: Stay Flexible
- Cake and sweets are okay in moderation: Your child can enjoy a small piece of cake or a few bites of dessert, especially if their blood sugar is stable and they’ve had a balanced meal earlier.
- Encourage movement: Kids usually run, dance, or play at parties, that physical activity helps balance out small sugar indulgences naturally.
- Check blood sugar if needed: Teach your child that it’s okay to pause and check, it’s part of self-care, not something to hide.
🫶 After the Party: Keep It Positive
• Talk it through: Ask how your child felt, were they comfortable, did they enjoy themselves, did they feel different? Listening builds trust and confidence.
• Avoid guilt: If blood sugar fluctuates, don’t make it a big deal. Use it as a learning moment and adjust next time.
💬 The Takeaway
Children with diabetes deserve to enjoy the same joyful moments as their peers. With planning, education, and open communication, birthday parties can be fun, safe, and empowering experiences that teach kids balance, not restriction.

👨👩👧 Parents as Role Models: What You Can Do
Children learn best by watching, and parents are their most powerful teachers.
Your everyday actions show that healthy living isn’t about rules or restrictions, but about balance, energy, and care.
💡 Lead with example:
- Eat balanced meals together and involve your child in choosing or preparing food.
- Make physical activity a fun family habit; walks, dancing, biking, or playing outside.
- Prioritize rest and stress management, as both deeply affect blood sugar and mood.
- Create a home where healthy choices feel natural, not forced.
- Focus on well-being and vitality, not body image or fear.
Most importantly, remind your child that diabetes doesn’t define them; it’s just one part of their story.
Encourage them to dream, play, and explore with confidence.
🌱 With love, patience, and consistent guidance, children with diabetes can thrive anywhere, at home, in school, and beyond.

💬 Final Thought
💡 Insulin is not our enemy, it’s our ally!
Our role is to create the right environment for it to work, balanced meals, daily movement, quality rest, and mindful care.
When we understand how the body functions, prevention becomes an act of empowerment, not fear.
💙 Because awareness, education, and compassion are the true foundations of lasting health.
📚 References & Further Reading
- World Health Organization (WHO) – Diabetes Fact Sheet
https://www.who.int/news-room/fact-sheets/detail/diabetes
→ Overview of diabetes types, symptoms, complications, and global data. - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Insulin Resistance & Diabetes Basics
https://www.niddk.nih.gov/health-information/diabetes
→ Explains how insulin works and what happens when it doesn’t. - American Diabetes Association (ADA) – Understanding Insulin
https://diabetes.org/health-wellness/diabetes-basics/insulin-basics
→ Details insulin’s roles, effects, and management of Type 1 and Type 2 diabetes. - International Diabetes Federation (IDF) – Type 1 & Type 2 Diabetes in Children and Adolescents
https://idf.org
→ Covers causes, management, and prevention strategies for pediatric diabetes. - Centers for Disease Control and Prevention (CDC) – Diabetes and Children
https://www.cdc.gov/diabetes/basics/children.html
→ Early signs, management at school, and family support. - Harvard Health Publishing – Why Type 2 Diabetes Is Now Affecting More Children and Teens
https://www.health.harvard.edu/blog/
→ Explains the growing prevalence of Type 2 diabetes among younger populations. - Harvard T.H. Chan School of Public Health – Nutrition and Diabetes Prevention
https://www.hsph.harvard.edu/nutritionsource/diabetes/
→ Evidence-based dietary recommendations for blood sugar control and insulin sensitivity. - World Health Organization (WHO) – Healthy Diet Fact Sheet
https://www.who.int/news-room/fact-sheets/detail/healthy-diet
→ Global guidelines for balanced nutrition and prevention of noncommunicable diseases. - ADA – Nutrition Therapy for Adults With Diabetes or Prediabetes (2023 Consensus Report)
https://diabetesjournals.org/care
→ Practical guidelines on meal planning, carbohydrate quality, and glycemic index. - Harvard Health Publishing – The Importance of Meal Timing for Metabolic Health
https://www.health.harvard.edu/
→ Discusses how late-night eating and circadian rhythms affect blood sugar regulation. - National Library of Medicine (NIH, PubMed) – Effects of Intermittent Fasting on Glucose Regulation and Insulin Sensitivity (review articles, 2018–2023)
→ Confirms that fasting can improve insulin sensitivity but must be medically guided. - NIDDK – Preventing Diabetes Complications
https://www.niddk.nih.gov/health-information/diabetes/prevention-diabetes-problems
→ Details on neuropathy, retinopathy, nephropathy, and heart disease prevention. - ADA – Standards of Care in Diabetes 2024
https://diabetesjournals.org/care
→ Comprehensive review of screening, treatment, and complication management. - JDRF (Juvenile Diabetes Research Foundation) – School and Diabetes Resources
https://www.jdrf.org/t1d-resources/life-with-t1d/school/
→ Guidance for teachers, parents, and caregivers on supporting children with diabetes at school. - Diabetes UK – Emotional Wellbeing and Diabetes
https://www.diabetes.org.uk/guide-to-diabetes/emotions
→ Tips for emotional and social adjustment for children and families. - National Institute for Health and Care Excellence (NICE, UK) – Type 1 Diabetes in Children: Diagnosis and Management
https://www.nice.org.uk/guidance/ng17
→ Comprehensive guidance on supporting children in home and school settings. - National Institute on Aging (NIA) – Alzheimer’s Disease, Insulin Resistance, and Brain Health
https://www.nia.nih.gov/health
→ Overview of the link between metabolic disorders and cognitive decline. - Journal of Alzheimer’s Disease (2018–2024) – Insulin Resistance as a Contributing Factor to Alzheimer’s Pathophysiology
→ Explores the concept often referred to as “Type 3 Diabetes.” - CDC – Gestational Diabetes: Risk and Management
https://www.cdc.gov/diabetes/basics/gestational.html
→ Evidence-based prevention and postpartum recommendations. - Mayo Clinic – Gestational Diabetes Overview
https://www.mayoclinic.org/diseases-conditions/gestational-diabetes/
→ Practical information for pregnant women and new mothers. - IDF Kids & Teens Program – Resources for Families Living With Diabetes
https://kids.idf.org - Beyond Type 1 Foundation – Practical Tips and Emotional Support for Families
https://beyondtype1.org